Students at Bob Jones University have created a non-profit company that provides tools to quickly detect malnutrition early and work with local officials to take swift action.
On Nov. 30 the student-created company Huruma Health sent prototypes of its system to Ghana for field testing in partnership with BJU’s Center for Community and Global Health.
Huruma Health, named for the Swahili word for compassion, began as a project for Global Challenges, a class offered each fall, which seeks to help students gain experience creating real-world solutions to current issues. Last year’s team won a $100,000 grant from Elon Musk’s XPRIZE Foundation and subsequently turned their idea into a business.
This year’s class focused on malnutrition. “We’re currently doing a nonprofit because we think it fits the goal of the organization the best,” said Emily Hughes, a senior business administration major on the team. Class member majors also include engineering, health care administration and public health.
Need of early detection
The team created the device primarily as an early detection tool for public health rather than as a clinical diagnostic tool, although it can be used in both settings.
Ghana experiences very high malnutrition. For children under age five, nearly one-fifth are stunted, and one-tenth are underweight for their age, according to the United Nations Children’s Fund.
The first 1,000 days in a child’s life are critical to healthy development, said Dr. Bernard Kadio, a professor in the Division of Health Sciences and one of the professors teaching the class. Furthermore, medical personnel can use simple body measurements to ensure that children are developing at a healthy rate.
“Within those 1,000 days, all those anthropometric measurements are basically the same,” Kadio said. That is, all healthy human babies grow at a constant rate in that time, within a well-defined margin.
Current methods in Ghana to detect malnutrition rely on schools collecting data in paper reports which are often not reviewed for several months, a time during which the child could slip deeper into health problems.
one case the team referenced, individual health reports for 5,000 children sat for three months before anyone reviewed them.
To eliminate this gap, the team designed and built a device called the Nutrition Screening Device, or simply Nutrimeter, which uses automatic data collection to simplify the collection process and provide instant results. The system uses a scale and a laser that records the child’s height reading on a stadiometer to send data directly to a computer with health measurement software.
“This is the beauty of the device,” Kadio said. “You have immediate nutritional information about the child,” allowing officials to immediately take action to help children at risk, he said.
The software shows where a child’s body mass index and z-score fall relative to healthy children, using a green-yellow-red display. In healthcare, z-score compares a person’s weight and height to the average for people of that age, with a zero representing the mean. A yellow result tells parents and providers that the child has a window of opportunity to get back on track but needs immediate intervention.

Photo: Derek Eckenroth (Derek Eckenroth)
Hopefully, team members say, Huruma will work with other nonprofits to provide its products for free or at very low cost. The team also created a paper resource called the Nutrition Status calculator, or Nutrislide, that can be used separately in doctor’s offices and classrooms to assess children’s growth. Field testing and future development
Although the project began as a class assignment, the team wants to continue their work beyond college. The class members are excited their project is already in real-world use in Ghana and they have many plans for improvements. They expect many suggestions to come from field testers using the device.
Team members have also designed an upgraded product model and created a list of improvements to make on future product versions.
First, they want to create better data analysis software. The current system works only on computers and has limited features. Other upgrades include adding tablet functionality for users without a computer and Bluetooth capability to the scale and stadiometer to reduce wires.
Eventually Huruma Health hopes to add capability to show z-scores for people beyond the age of 5 and offer an app and expand its website (hurumahealth.com) to offer the NutriMeter and NutriSlide and a contact form.
Though the team originally intended to run the company as a Limited Liability Company and started an LLC, which they can still use to protect their intellectual property, the students plan to run Huruma Health as a non-profit company. The company will have a board of trustees, comprising the original team members, who will appoint officers to oversee the work on the ground. The team plans to hire a business intern as project manager next semester.
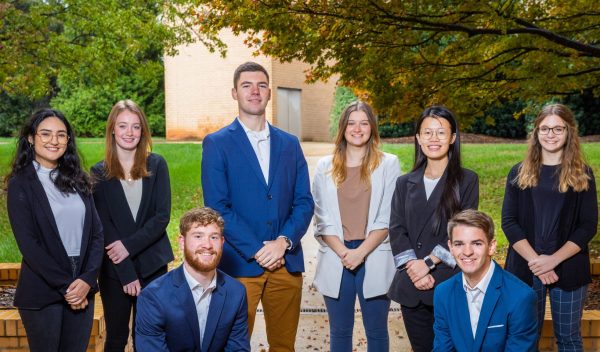
This semester’s Global Challenges class is taught by Dr. Bill Lovegrove, head of the department of engineering, Dr. Adele Dunn of the Division of Management, Dr. Amy Hicks, chair of the Division of Health Sciences and Dr. Kadio. The students are Hughes and accounting major Mark Dickerson; engineering students Jiayi Lin, Debanhi Flores and Andrew Taylor; and health science students Jonathan Du Fault, Deeanna Perry and Paige Williams. All the students are seniors aside from juniors Perry and Lin.
The team presented their research and product at a forum in Levinson Hall on Nov. 30. Field testing wrapped up on Dec. 8.